Several changes in the nails or toenails might lead individuals to believe they have tinea unguium, formally referred is onychomycosis, a fungal nail infection. Sometimes a fungal disease of the fingernails makes an illness seem infectious or connected to lousy hygiene. In reality, 10 percent of all individuals in Western nations develop fungal nail infections, and adults 60 and older represent a 20% rise in this proportion. Compared to fingernails, talon fungus is far more prevalent. In truth, various illnesses, including, yet not restricted to, a fungal infection, may cause unusual-appearing nails. Your nails may have a varied appearance for a variety of additional reasons.
How can you remove talon fungus?
Maintaining well-groomed and filed nails are strongly advised as this might lessen the number of fungi in the nails. When thicker nails produce pressure-related pain, this also relieves the discomfort. Oral drugs have been more successful in treating nail fungus than creams and other topical therapies, and this is because external applications cannot penetrate the hardness of nails. Maintaining a schedule for topical medications is also tricky. These drugs often need to be taken daily for up to a year to show effectiveness. Compared to oral treatment, the lower likelihood of significant side effects and medication interactions is one of the topical therapy’s main benefits.
The following are topical prescription drugs for fungal nails:
Lacquer ciclopirox: In persons with healthy immune systems, the medical nail lacquer ciclopirox (Penlac) external solution 8% has been authorized to treat toenail or finger fungus that does not affect the white part of the nail (lunula). In one research, ciclopirox was 22% effective in eliminating the fungus. Once every day for up to a year, the drug is given to the damaged nails. Once a week, the lacquer has to be cleaned with alcohol.
Amorolfine external solution 5%: There’s some proof that applying an antimicrobial nail lacquer with amorolfine helps stop reinfection after a cure, with an effectiveness rate of roughly 70%. The U.S., however, does not presently have access to this medication.
Efinaconazole (Jublia): In 2014 saw the approval of the drug efinaconazole (Jublia). Because the two most prevalent fungal species that affect nails are topically (applied to the skin), it is an antifungal used locally for treatment. For 48 weeks, you must apply once per day. Ingrown toenails, dermatitis at the application site, and discomfort are the most frequent adverse effects of Jublia.
Tavaborole (Kerydin): Another brand-new drug treating onychomycosis of the toes is tavaborole (Kerydin). This drug treats the same medical condition as efinaconazole. Additionally, 48 weeks of daily application are necessary. Similar to Jublia’s common side effects, Kerydin has them as well.
What other diseases or illnesses resemble fungal nails?
In place of fungal nails, you can also have one of the following conditions:
Ridges and lines are common and could even be regarded as usual, and they might worsen during pregnancy. A deep groove down the center of the nail may develop due to nail biting. After chemotherapy, some people could experience these alterations.
Senile fingernails: Your nails become more fragile with age, develop ridges, and the sections at the tip begin to separate. To avoid this, use clean solutions, and stay away from soaking the nails in water.
Yellowish or white nails may occur from onycholysis. This defines the separation of the nails from the toenail. You can make out the color of the air beneath the nail. The suggested treatment is trimming the nail without sanitizing underneath, adding polish unless you want to hide the coloration, and waiting two to three months. The risk of fungal infection may increase after onycholysis.
Trauma often leads to hematomas or blood under the nail, which causes black or red nails. As the fingernail grows, the discolored area will appear alongside it and be trimmed away when you trim your nails. If you notice a black spot under your nails that wasn’t caused by trauma or if it involves a toenail, you might need to visit a dermatologist or get a pedicure to be sure it’s not melanoma. Fast biopsies may detect cancer (cancer).
Pseudomonas bacteria that develop beneath a telcon that is only partly detached from the telcon bed might result in green nails, and the infection might make the nails smell bad. The recommended course of action is to clip your nails short regular four weeks, avoid cleaning them, and only polish them if you wish to cover up the color and see for three months. Additionally, it is advisable to dry the fingernail after a bath fully and to prevent immersing it in any liquid (even if it is done while wearing gloves). Your doctor could attempt several pharmaceutical remedies if the issue persists.
Psoriasis and other skin conditions that impact the telcon matrix, the area right beneath the epidermis beyond the nail, may be indicated by pitted telcos. This is where the nail starts to grow. Tan nails may also be a side effect of psoriasis-related nail discoloration.
The swelling and inflammation of the epidermis around the nail are referred to in medicine as paronychia. This is an epidermal infection near the bottom of the telcon (cuticle). Bacteria often cause acute disorders that appear fast. Warm baths could be helpful, but the fluid will need to be routinely drained by a doctor. Chronic paronychia develops when a cuticle becomes inflamed or disturbed over time. Occasionally, yeast may spread infection on the weaker skin by taking full advantage of it. The initial stage of treatment is to maintain the skin’s dryness and keep it out of water. Contacting a doctor is advised if the problem continues. Despite their rarity, antibiotics could be necessary for situations of serious illness.
Chronic telcon stress from starting and often stopping, kicking, and other athletic activities may damage the nails and cause them to resemble fungus. A recurrent injury might also be brought on by specific vocations or leather footwear. Some events may leave you with long-lasting alterations that mimic fungal telcon.
Reason for the are the risk factors for fungal telcon and their cause?
The most frequent cause of fungal diseases of the nails in healthy, average persons is a fungus that thrives in damp, wet environments. Communal showers in gyms and swimming pools are typical sources. Other risk factors include living near relatives with fungal nails and frequent nail salons that do not adequately sanitize tools. There is evidence that athletes are more prone to nail fungus. This is thought to be caused by the frequent stress on the toenails caused by wearing sweaty, tight-fitting shoes—the fungus’s likelihood of infecting your toenails increases if you have an athlete’s foot. Repetitive damage weakens the nails, which increases their susceptibility to a fungus infection.
Additionally, more vulnerable are the elderly and those with certain underlying diseases. Your susceptibility to contracting the fungus may be increased by anything compromising your immune system. AIDS, cancer, diabetes, psoriasis, and any immunosuppressive drugs like steroids are a few examples of these.
Are nail fungi contagious?
Even though the fungus should be acquired from somewhere, it is not very infectious. Since it is so widespread, it is seldom a chance to discover more than one individual in a family suffering from nail fungus. It can only be passed from one person to another through ongoing close contact.
What is the remedy for fungus-ridden nails?
The survival of patients for orally antifungal therapy varies depending on the medication. Treatment might take nine to twelve months before you tell if it was effective because of how long the fingernail takes to grow out. Even with successful therapy, the fungus may come back. Oral antifungal medicine is the best treatment for nail fungus since it has a higher-excellent cure rate and a short processing period than topical therapy.
The following oral prescription medicines are effective against telcon fungi:
Grifofulvin has long been the mainstay of oral antifungal therapy (Fulvicin, Grifulvin, Gris-Peg). This medicine is secure, and it is ineffective for treating toenail fungus. Lengthy results have reportedly proven underwhelming, and newer medications have substantially taken their place.
Terbinafine (Lamisil) is used daily for twelve weeks for nails and six weeks for fingernails. The drug is safe and effective with a low incidence of side effects, and it should be used with caution in patients with liver disease. This medication is very reasonably priced.
Pulse dosages of the drug itraconazole (Sporanox) are often administered. It could interact with several widely used medications, such as antibacterial erythromycin and asthma medications. This treatment is believed to be effective for onychomycosis caused by the Candida fungus, plus no dermatophytes mould.
For a few months, fluconazole (Diflucan) may be used weekly. The dose of this medicine may have to be adjusted if the individual has a weak renal function or is taking it at the same time as a few other medications. Because it isn’t as effective as Sporanox or Lamisil, individuals with liver disease should use it cautiously.
A specialist will decide if a quick blood test is necessary to screen for liver illness.
Many novel therapies are even being used for testing, including:
A light-activated substance is applied to the nail during laser treatment or photo-dynamic then the nail is exposed to the light of the appropriate wavelength.
Iontophoresis uses an electrical charge to facilitate the nail’s absorb properties of topical nail fungal infection cream India.
Use a specialized nail that modifies the nail’s microclimate to make it unfavorable for the fungi to develop: If this succeeds, it might be a low-cost solution to handle this issue in the time ahead.
Surgery is one method of permanently eliminating toenail fungus. Nail removal is a surgical procedure for onychomycosis. Without concurrent use of additional antifungal medicine (oral or topical), this at times only offers temporary relief, and repetition is frequent. The afflicted nail may need to be surgically removed if additional causes like infection or trauma are present.
For talon fungus, are there OTC remedies?
OTC goods may be purchased at a regular retail store without a doctor’s prescription or license. Even though there aren’t many over-the-counter drugs (OTC) available to treat fungus nails, many lack U.S. approval due to a lack of testing. Onychomycosis therapy is regulated by the Drug and Food Agency (FDA). Most over-the-counter medications treat fungal infections that affect the skin, not the talons. Few drugs feature propylene glycol and undecylenic acid as their primary component. These chemicals prevent fungal development, but they might not sufficiently enter the fingernail to be helpful in the treatment of fungal nails.
Suggestions for preventing fungal nails
Only 50% of abnormally looking nails are caused by nail fungus. It might be challenging to distinguish between the several reasons for discolored fingernails. The disease Onychomycosis is rarely treated. Indications for therapy include
- Obesity,
- Prior infection in the legs,
- If you experience any problem or feel discomfort because of your nails,
- You want them to have treatment for good reasons.
Recurrences and failures of treatment are frequent.
The key lies in prevention. The following precautionary steps might be beneficial:
- Try Keeping your fingernails short, and avoid going too far into the sub corner while trimming them.
- Keep the feets hygenic and completely dry them.
- Wear loose-fitting shoes and dry socks.
- Switch up your athletic footwear.
- Refrain from using solid cleansers or soaking your hands in water.
- Address the athlete’s foot as soon as it appears.
Is it feasible to halt fungal nail growth?
The fungus is everywhere, so no one can pinpoint where a special individual contracts it. However, there are several spots one should avoid or utilize cautiously since the fungi grow in warm, damp regions. No research supports the theory that the fungus may be found on shower floors, lockers, and swimming pools. Additionally, nail paint and artificial nails reduce the nail’s ability to breathe, increasing the risk of a fungus infection. There are fungi in the earth, the air, and on everything. Spraying socks and other footgear as part of hygienic procedures seems reasonable and could be helpful. However, the most significant possible protection may be to refrain from wearing tight, non-breathing shoes or to avoid walking on the floors of sporting facilities. Nail fungus may be avoided by daily foot washing and between-toe drying. Nail fungus is not often brought on by the fungi that live on the hairs of pets like cats and dogs. White socks are not helpful.
Conclusion
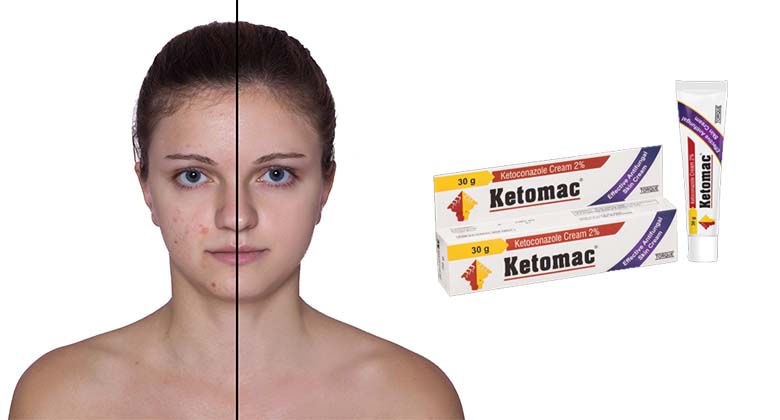
In conclusion, now is the time to research high-quality antifungal nail polish in India and try it. You never know what will cure you the best; sometimes, the solutions are elementary! One of the companies is Ketomac, renowned for its antifungal cream for nails in India that treat the side effects of fungus nail infections and may be used on lips as well. It aids in reducing the adverse effects of burning, itchiness, redness, peeling, and drying of the nail.